#HAWMC Day 9.
Share with readers about a time you had to overcome a daunting challenge. What words of encouragement would you share with others who find themselves facing similar difficulty?
I’ve written about diagnosing myself with a prolactinoma. This post will be about how I decided on the course of treatment.
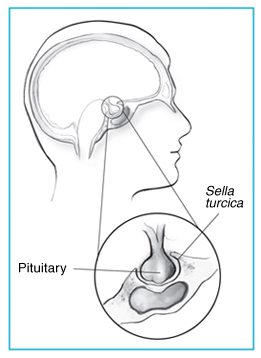
When I diagnosed myself in the year 2000, I was Chief Resident of internal medicine. I hadn’t taken endocrinology training yet. I asked an endocrinologist about my case informally. I showed my MRI. The advice was to undergo surgery to remove the tumor. So I went to a neurosurgeon. My pituitary tumor had a cystic part. It also had a suprasellar component – that meant part of it was sticking above the sella.
The approach to removing the pituitary tumor is called a transsphenoidal excision (TSE). Yup, like you can see in the picture, it involves going through the nostril and drilling through the bone to get to the pituitary gland. Ordinarily, the neurosurgeon told me, that the portion of tumor sticking above the sella (suprasellar) cannot be reached via this method. But since my tumor had this cystic portion, it would likely collapse and be “suckable.” I didn’t like the sound of that. I wondered about my normal pituitary cells and how they could be sucked into oblivion!
Photo credit: http://neurosurgery.ufl.edu/patient-care/diseases-conditions/pituitary-tumors/
I was single but in a relationship then. I worried about my fertility after surgery. Will I end up worse off, with hormonal deficiencies?
I was also vain! I worried what would happen to my nose. Will it still look the same after a TSE? I asked my neurosurgeon that and he laughed. He told me he could do the sublabial technique with an incision below the upper lip and avoid going through the nostril altogether. I plucked up my courage to ask him how many of these procedures he had done. He said, fifty. I wasn’t convinced!
I told my parents. They didn’t have medical backgrounds. They said they would support me, if I chose to undergo surgery. The decision was squarely on my shoulders. Part of me wished it wasn’t so.
I learned about evidence-based medicine in residency. I even attended an advanced EBM workshop. I didn’t know I would have to do an evidence-based evaluation of my own options for managing a prolactinoma. I spent nights scouring PubMed.
In the end, I decided to try bromocriptine. My neurosurgeon didn’t like that. He said that taking bromocriptine would make the tumor more fibrotic and harder to remove later on. But I thought, First do no harm. The tumor might still respond with bromocriptine.
And that’s what I did. In the year 2000, both surgery and bromocriptine were recommended for prolactin-producing pituitary tumors. Later guidelines though favored medical treatment with bromocriptine.
A few years after my diagnosis, I ran into my neurosurgeon in the hospital elevator. He asked me how I was. I told him I had my first son and I was doing well. He said, I’m glad you decided to take bromocriptine. The guidelines now say medical treatment is preferred.
So what advice can I give after this experience?
If you’re a patient faced with a difficult medical decision, try to learn as much as you can about your condition. The doctors can give you the options but in the end, only you can decide about the course of treatment.
Granted, I am not the typical patient. I was a physician in training. But I didn’t feel confident at all at first deciding on what to do, even for myself. Let me end by referencing some advice from Martine Ehrenclou in her book, The Take-Charge Patient –
- Become your own advocate
- Choose the best doctor
- Communicate effectively with doctors
- Prepare for your medical appointment